A 64 year old male with vomitings and right flank pain
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Then 3 yrs later he developed a midline swelling approx 3 cm below umbilicus and diagnosed with abdominal hernia and a mesh was placed.
Then 1 yr later he developed abdominal pain and endoscopy was done and diagnosed with ulcer and was managed conservatively During this he was diagnosed with diabetes and hypertension
Then 2 yrs back he developed generalized weakness and went to hospital and was told that haemoglobin (6 g/dl)was low and was given iron injections.For which he went to Hyderabad orange hospitals and because of financial crisis he came to KIMS Narketpally .
Patient presented to KIMS opd 12 days back .
Since 15 days patient has complaints of vomitings 3-4 times per day containing of food contents in it . Non bilious , non projectile. Not associated with fever , malaise , headache .
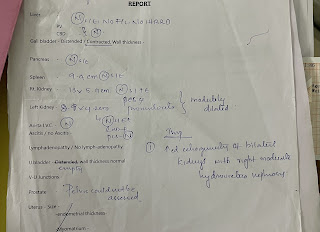
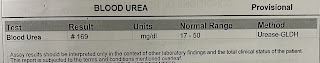
Right sided lower flank pain which dull aching type of pain radiating to the front in the lower right quadrant ( loin ) associated with Burning micturition and slight pain since 15 days . History of reduced urine output .
DAILY ROUTINE:
Patient wakes up at 5 am and takes breakfast at 7 and lunch around 12pm and dinner at 8pm and rest of the time spends time with grandchildren. His daily routine is not disturbed even after having illness.
PAST HISTORY-
History of similar complaints in the past .
DM and Hypertension since 7 years .
No history of asthma , epilepsy, CAD , TB
FAMILY HISTORY - no significant family history
DRUG HISTORY- no history of drug allergy
PERSONAL HISTORY-
Diet- mixed
Appetite- decreased
Sleep- adequate
Bowel and bladder- burning micturition and decreased urine output
Addictions- alcohol occasionally
GENERAL EXAMINATION-
Patient is conscious, coherent and cooperative
Moderately built and nourished
Pallor - absent
Icterus- absent
Cyanosis- absent
Clubbing- absent
Lymphadenopathy- absent
Edema- absent
VITALS -
Temperature- a febrile
Pulse rate - 86 bpm
Respiratory rate - 17 cpm
BP - 90/60 mm of hg
SYSTEMIC EXAMINATION-

















Comments
Post a Comment