A 49 year old male with chest pain
15 Feb 2022
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This Elog book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment .
Patient and his/her attenders have been informed and their consent has been taken.
A 49 YEAR OLD MALE PATIENT WHO IS TODDY TREE CLIMBER BY OCCUPATION CAME ON SATURDAY TO OP WITH
CHEIF COMPLAINTS OF -
Severe chest pain since 5-6 days
Fever and Cough since 5-6 days and
Shortness of breath since one day
HISTORY OF PRESENTING ILLNESS-
Patient was apparently asymptomatic 1 week back then he developed fever which was high grade along with chills and rigor which relieved on medication.
He also has yellowish discolouration of sclera .
He developed dry cough after he got fever . Chest pain aggravates on coughing since 2 days .
History of (1 episode) vomiting when he had fever . Which was watery and had food particles in it . Non bilious
Patient presently complains of chest pain which is aggravating on coughing and while talking along with shortness of breath since 2 days .
Patient had similar complaints of fever with chills and rigor 4 years back when he was diagnosed to have DM along with fatty liver and jaundice.
He has history of seizures since last 5 years .
5-6 episodes in last 5 years .
Last episode was 1 year back .
FEVER CHART
PAST HISTORY -
Diabetes Mellitus - since past 3 years
No history of BP , TB , Asthma, thyroid abnormalities .
FAMILY HISTORY-
No significant family history.
PERSONAL HISTORY-
Appetite- decreased
Diet - mixed
Sleep- inadequate
Bowel and bladder- regular (now)
Addictions- Chronic Alcoholic
Chews Tobacco
Chronic alcoholic- as he takes 1/2 bottle of whiskey daily since last 20 years .
GENERAL EXAMINATION-
Pallor - present
Icterus- present
Cyanosis - absent
Lymphadenopathy- lym
Edema - absent
SYSTEMIC EXAMINATION-
CVS-S1 and S2 heard
CNS-no abnormalities detected
Respiratory-bilateral air entry is present
Per abdomen- soft , non tender
INVESTIGATIONS-
ECG-
HEMOGRAM
Hb- 11.6gm%
TL-17,700 cells/cubicmm
Neutrophils-87%
Leukocytes-10%
PCV-31.8
MCHC-36.5
RBC-3.7millions/cubic mm
PLT-1.6 lakh
LIVER FUNCTION TEST
Tb-3.13
Db- 1.47
SGOT-27
SGPT-15
Alk Phosphatase - 225
TP-5.3
Alb-2.61
A/G-0.97
COMPLETE URINE EXAMINATION
Sugars- present
Albumin- trace
Pus cells - 2-3
E. Cells - 3-4
Rbc- nil
KETONE BODIES- present •
BLOOD SUGAR-
RBS- 418
FBS- 269
PLBS-
HbA1C- 8.2
SERUM AMYLASE- 26IU/L
SERUM LIPASE- 17IU/L
ULTRASOUND
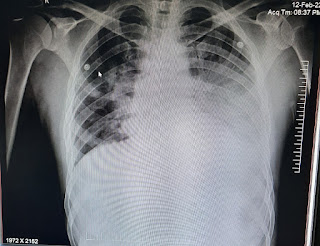
CHEST X-RAY-
PROVISIONAL DIAGNOSIS
TREATMENT-




















Comments
Post a Comment