A 46 year old male presented with seizures to the hospital
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
20/07/2022
Blog by Janhavi Virani
Roll no 58
46 year old male patient who is Presser by occupation resident of Miryalguda brought to casuality with chief complaints of
— recurrent episodes of seizures since the day before
— pain and swelling in right shoulder
Patient was apparently asymptomatic 12 years back then he had his first episode of seizure , 6 months back he had 2nd episode of seizure, 2 days before presenting to opd he had 2 episodes and the day before he came to opd he had 8 episodes of seizure.
He presented with recurrent seizures abrupt in onset , each episode is associated with bilateral upper and lower limb spasms, up rolling of the eyes , tongue biting and state confusion after episode.
Tongue biting is associated with bleeding.
Each episode lasting for 1 to 5 mins .
Occurrence of seizures is after alcohol consumption , tobacco consumption, strenuous
Not associated with aura , salivation , involuntary defecation and micturition.
During Recurrent seizures —> patient fell down which led to dislocation of the right shoulder went to nearby government hospital and was referred to Kims .
He had sudden onset of pain in shoulder which is Dragging type associated with swelling and bluish discolouration is skin around the shoulder
No history of fever , headache , trauma , vomitng ,
Above history is explained by patient’s attendant . She is reliable.
Past History-
No history of Diabetes Mellitus , Hypertension, asthma, tuberculosis, CAD
12 years back he went through surgery for injury to right hand in which his little and right finger of right hand was amputated .
Family History-
No significant family history .
Personal History -
Diet : mixed
Appetite : normal
Sleep : adequate
Bowel and bladder: regular
Addictions :
History of alcohol consumption since 25 years - 25 units / day since 20 years .
History of tobacco consumption since 25 years - 5 packets / day
GENERAL EXAMINATION -
Patient is conscious, coherent, and cooperative
Well built and moderately nourishment.
Pallor - absent
Icterus- absent
Cyanosis - absent
Clubbing- absent
Edema - absent
Generalised lymphadenopathy-
Vitals -
PR - 70 bpm
RR - 16 cpm
BP - 110/80 mmHg
Temperature- a febrile
SYSTEMIC EXAMINATION-
Cardiovascular system
JVP - not raised
Visible pulsations: absent
Apical impulse : left 5th intercostal space in midclavicular line.
Thrills -absent
S1, S2 - heart sounds heard
Pericardial rub - absent
Respiratory system:
Patient examined in sitting position
Inspection:-
oral cavity- Normal ,nose- normal ,pharynx-normal
Shape of chest - normal
Chest movements : bilaterally symmetrically reduced
Trachea is central in position.
Palpation:-
All inspiratory findings are confirmed
Trachea central in position
Apical impulse in left 5th ICS,
Chest movements bilaterally symmetrical
AUSCULTATION
BAE+, NVBS
Abdomen examination:
INSPECTION
Shape : normal
Umbilicus:normal
Movements :normal
Visible pulsations :absent
Skin or surface of the abdomen : normal
PERCUSSION- tympanic
AUSCULTATION :bowel sounds heard
CNS -
Higher mental function -
patient is conscious
oriented to time place and person .
Emotionally stable
Speech : comprehension is normal , fluency is reduced as he had history of tongue biting during his episodes of seizures .
Emotionally stable
CRANIAL NERVE EXAMINATIONS - no abnormalities detected
Motor system examination-
Power Left
Upper limb 5/5
Lower limb 5/5
Tone. Left
Upper limb Normal
Lower limb Normal
Reflexes - done only on left hand
Bicep
Tricep
Knee
Ankle
PROVISIONAL DIAGNOSIS-
Status Epilepticus with Right shoulder dislocation.
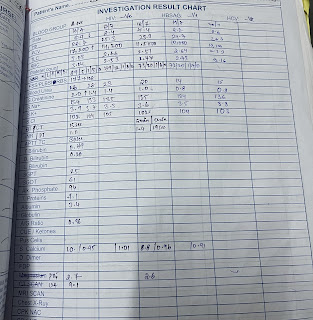
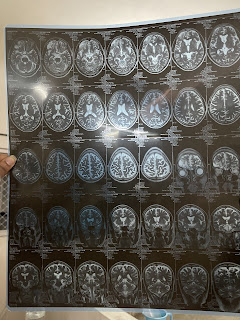
INVESTIGATIONS-
ECG
MRI Brain
TREATMENT-
Inj Levipil 500mg iv/bd
Inj Thiamine 200mg
Inj Monocef 1gm iv/bd
Inj PAN 40mg iv
Inj ZOFER 4mg iv












Comments
Post a Comment